Endocrine Disorders
• Anterior Pituitary: (ACTH, TSH, FSH, GH, LH, Prolactin)
– Hypo: Hypopituitarism
– Hyper: Hyperpituitarism
• Posterior Pituitary: (Oxytocin, ADH)
– Hypo: Diabetes Insipidus
– Hyper: SIADH
• Adrenal Cortex: (Gluco/Mineralcorticoids, Androgens)
– Hypo: Adrenal Insufficiency (Addisons and Addisonian Crisis)
– Hyper: Cushings Syndrome and Hyperaldosteronism
• Adrenal Medulla: (Catecholamines; Epi/Norepi)
– Hypo: Adrenalectomy can cause s/s of hypo secretion of cortex & medulla
– Hyper: Pheochromocytoma
• Thyroid
– Hypo: Hypothyroidism and Myxedema coma
– Hyper: Hyperthyroidism and Thyroid storm
• Parathyroid
– Hypo: Hypoparathyroidism
– Hyper: Hyperparathyroidism
• Pancreas
– Diabetes Mellitus: Type 1 & Type 2
• Complications: Retinopathy, Nephropathy, Neuropathy
– Diabetic KetoAcidosis (DKA)
– Hyperglycemic Hyperosmolar Nonketotic Syndrome
We are going to concentrate on the most frequently covered topics on the NCLEX exam:
Thyroid, Adrenal, and Parathyroid disease, as well as Diabetes and all of it's complications.
But first, keep in mind these Key Points:
• Only 2 things can happen: Hypo or Hypersecretion of an endocrine organ
• Treatment is aimed at blocking (if hyper) or replacing (if hypo) hormones
• Primary disease is due to a dysfunction in the gland itself, while Secondary is due to a dysfunction in the glands' stimulating hormone.
• Look out for Meds, Hi yield points, and Precautions
Thyroid Disorders
Hypothyroidism
• 1o: Surgical resection, Amiodarone, Low Iodine, Hashimotos
– Hashimotos: Autoimmune destruction, usually in women 20-60 y.o.
• 2o: Hypothalamus or Pituitary disorders
• S/S:
– Early: Fatigue, cold intolerance, wt gain, dry skin, brittle hair/nails, hi DBP
– Late: Slow speech, hoarse, loss of outer 1/3 eyebrow, myxedema (thickened skin), periorbital puffiness, low HR, effusions
– Critical (Myxedema Coma): Low Temp, Low BP, Low R, AMS
• TX: Levothyroxine (Synthroid)
– Myxedema Coma: T4 IV (can use T3 if T4 ineffective but CX for arrhythmias); Adrenal replacement meds (steroids) usually necessary
Hyperthyroidism
• 1o: 3/4 of all hyperthyroidism is Graves; Goiter, Adenoma, and Amiodarone also cause
– Graves: Autoimmune induced, usually in women 20-40 y.o.
• 2o: Pituitary adenoma
• S/S:
– All: Insomnia, heat intolerance, wt loss, sweaty, fine hair, hi HR, AFib, incr. bowel movements
– Graves: Above + non-tender goiter, pretibial myxedema, exopthalmos
– Storm: Fever, hi HR, hi SBP/Wide pulse pressure/ low MAP (i.e. 150/40) CX: 50% MORTALITY!
• TX:
– 1o: Propranolol ( lowers HR and lowers T4/T3 conversion)
– 2o: PTU or Methimazole (antithyroid medications used as 1st line tx attempt prior to ablation of thyroid)
– 3o: Radioactive Iodine (Cat X drug used to diagnose nodules and destroy thyroid tissue; Highly radioactive so strict precautions are necessary, i.e. keep distance from pt when possible, tell pt to avoid close contact for 3 d after
– Storm: BB then PTU wait 1hr then Iodide then Steroids
Amiodarone: The Thyroid Killer
• Over 10% of those treated with Amiodarone will develop hypothyroidism
– Amio looks like Iodine = Thyroid takes it up instead of Iodine = can’t make T3/T4 = Hypothyroid (often resolves in 1-3 months)
– Some have antibodies that attack and destroy thyroid when combined with amio = Hypothyroid (nonreversible)
• Up to 20% of those treated with Amiodarone will develop hyperthyroidism
– Amiodarone has a special affinity for the thyroid and when it accumulates there, tissue becomes hyperemic, allowing pre-formed T3/T4 to dump into bloodstream = Hyperthyroid (often becomes hypothyroid when supply is used up, then can normalize)
Adrenal disorders
Cushings
• Cushings Syndrome: Hi Cortisol from any cause
• Cushings Disease: Hi Cortisol from a Pituitary cause (2o)
• Iatrogenic Cushings: Prescribed steroids (most common cause)
• Ectopic Cushings: Lung CA can release an ACTH like hormone that causes Cushings
• Patho:
– Cortisol (Glucocorticoid) has the following effects on the body: Impaired collagen production,
Enhanced protein catabolism, Anti-insulin effect (hyperglycemia), Inhibitory effect on T-cells (Impaired immunity), Enhanced catecholamine activity (HT)
• S/S:
– Syndrome: Central obesity, moon facies, buffalo hump, purple striae on abdomen, acne, easy bruising, HT, Hi Glucose, Hi Na, Low K, Psychiatric issues
– Disease only (symptoms caused by faulty release of Melanocyte stim hormone during release of increased ACTH): Hyperpigmentation, Masculinization in females
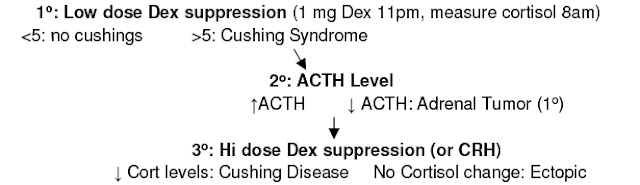
• Diagnosis: Dexamethasone suppression test
• TX: If Iatrogenic, taper steroids
– Disease: Transphenoid resection of tumor
– Adrenal: Adrenalectomy
Adrenal Insufficiency
• 1o: Addisons (autoimmune most common in 1st world, infection most common in rest); Only
type of insufficiency where aldosterone is also low
• 2o: Iatrogenic (Pts on long term steroids can not produce their own steroids when stressed or
upon abrupt withdrawal)
• S/S:
– All: Wt loss, anorexia, nausea, abdomen pain
– 1o: Low Aldosterone (Low Na, Hi K), Glucose, Orthostasis, Pigment (from Hi ACTH)
– Addisonian Crisis: Severe Low BP, Cardiac collapse, Ab pain, ARF; Crisis brought on by stress, trauma, or infection
• Fatal if untreated
• TX: IV fluids (min 2 L D5 NS) + Hydrocortisone
• DX: 1) Measure plasma Cortisol; If Low, check Plasma ACTH, Aldosterone, and Renin
Primary (addisons): Hi ACTH, Hi Renin, Low Aldosterone
Secondary: Low ACTH, Normal Renin/Aldo
• TX:
– 1o: PO Hydrocortisone or Prednisone QD + Fludrocortisone QD
– 2o: Same as above but no need for Fludrocortisone since no low mineralcorticoids in 2o
Pheochromocytoma
• Hi Catecholamines from Adrenal Medulla mass
• S/S: Very hi BP, pounding headache, severe sweating, anxiety, impending doom, hi glucose, hi K, Hi Lipids
• DX: Urine screen for metanephrine (an epi breakdown product), will be elevated; May also
check urine/serum epi/norepi levels; CT/MRI to detect location of mass
• TX: Alpha blockers, followed by surgical resection
Hyperaldosteronism
• Usually from Adrenal Cortex adenoma (Conn’s syndrome) or hyperplasia
• Patho: Aldosterone is the primary mineralcorticoid in the body that is responsible for saving
Na in the DCT/CD of the kidneys, thus preserving water and increasing volume; K is wasted
in exchange for Na; Responds to Renin; Fludricortisone is pharm version of this hormone
• S/S: hi Na, Low K, HT, Polydipsia, Polyuria, no peripheral edema, M.Alkalosis
• DX: Aldosterone/Renin ratio (Hi/Lo which shows Renin is not the cause of hi Aldo)
• TX:
– Hyperplasia: Spironalctone
– Adenoma: Resection
Steroids: Just so you don't get confused, here is a chart that shows which of the steroids we use in the hospital have solely Glucocorticoid effects, which have Mineralcorticoid effects, and their strength compared with the natural steroid Cortisol.
Pituitary disorders
SIADH
• Often hi ADH is seen after stroke, trauma or pain due to hi blood flow and release of hormone
• Iatrogenic: Meds (SSRIs, Morphine, Oxytocin) can also cause
• Lung: CA, pneumonia or TB can release an ADH-like hormone
• S/S: Low Na (free water retention) w/CNS changes (lethargy, falls, Sz, coma), low Renin,
hypervolemia, low BUN/Creatinine
• TX:
– 1o: Water restriction (usually sufficient)
– 2o: NS + Lasix if faster results desired
– 3o: Lithium or Demeclocycline inhibit ADH if severe; May also add Hypertonic saline if neuro s/s
– CX: NEVER raise Na more than 0.5 meq/L/hr (12/d) or will develop pontine myelinolysis
Diabetes Insipidus
• Central: Most common form, low ADH from surgery or head trauma
• Nephrogenic: poor response to ADH due to low K, hi Ca or Lithium
• S/S: Polyuria (5-15 L/d), clear urine, polydipsia, hi Na, low Urine osmolality , hi plasma osmol
• DX: DDAVP-if response you have both diagnosed and treated central DI
• TX:
– Central: DDAVP (Desmopressin-synthetic ADH/Vasopressin that is much stronger and longer acting), nasally, PO or injection; Chlorpropramide increases response to ADH
– Nephrogenic: Thiazide diuretics (block DCT Na uptake forces PCT to reabsorb Na and water, so less water reaches the faulty ADH channels)
Parathyroid disorders
Hypoparathyroidism
• Facts: Hyposecretion of parathyroid hormone, often following thyroidectomy
• S/S:
– Subjective: Numbness/Tingling in face, depression, Muscle cramps
– Objective:
• Hypocalcemia, hyperphosphatemia, Hypotension
• + Trousseau (BP cuff causes carpal spasms)
• + Chvostek (Tap facial nerve contracts face muscle)
• Hyper DTRs, Seizures
• Cardiac arrhythmias, Prolonged QT interval (Primary r/o with long QT)
• TX: Calcium gluconate (Serious: IV; Mod: PO); Vitamin D
• NX:
– Calcium and Vitamin D can increase Ca excretion = stones
– Initiate Seizure precautions
– Place Tracheotomy set, Oxygen, Suction at bedside
– Monitor for Tetany: s/s include arrhythmias, carpopedal spasm, dysphagia, cramping,
numbness/tingling in face/extremeties, + Chvostek/Trousseau, Seizures, Photophobia,
Wheezing/Dyspnea (Broncho/laryngospasm)
Hyperparathyroidism
• Facts: Hypersecretion of Parathyroid hormone
• S/S:
– Stones: Nephrolithiasis (Renal calculi/stones)
– Bones: Bone pain, Bone deformities, Pathological fractures
– Groans: Muscle pains/weakness, PUD, Pancreatitis, Gout, Constipation
– Psychiatric overtones: Depression, Anorexia/weight loss, lethargy
– Others: Hypercalcemia, Hypercalciuria, Hypophosphatemia, HT, Polyuria, Polydipisia, Shortened QT Interval
• TX:
– Furosemide (Lasix) to lower calcium levels by up excretion
– IV fluids of NS
– Calcitonin (Calcimar) to lower skeletal calcium release
• NX:
– Notify MD if rapid drop in Ca occurs and assess for s/s of tetany
Pancreas disorder
Diabetes Mellitus
• Facts: Inability to control blood glucose
• Type 1: Autoimmune beta islet cell destruction, usually presents as a kid, less than 10% of all DM
• Type 2: Insulin resistance = hi glucose = hi Insulin = pancreas fails = overt DM, more than 90% of DM
• S/S:
– Type 1: Develop hyperglycemia rapidly, often after illness, usually presents in DKA
– Type 2: Polyuria, polyphagia, polydipsia, frequent infections; May present w/comorbidities such as MI, stroke, claudication, neuropathy, proteinuria; often discovered on routine UA or sugar check
• DX: Diabetes; 4 independent methods
– more than126 after 8 hour fast (preferred method) (less than 110 norm)
– more than 200 at anytime w/DM s/s
– more than 200 2 hr after 75g oral glucose load (less than 140 norm)
– more than 6.5 hbA1C at anytime
• DX: Impaired glucose tolerance (not quite DM but hi risk of future development)
– 110 -126 after 8 hour fast
– 140 - 200 2 hr after 75g oral glucose load
– 5.8-6.5 hbA1C
• TX considerations:
– HbA1C: Gives an estimate of glucose control over previous 3 mos as it measures how many
hemoglobin are coated in glucose
• less than 5.8 (perfect); below 7% (ok); 7-8.5% (good); 8.5-10% (fair); above 10% (poor)
– Check sugar/Administer Insulin 4x/d: qmeals and qhs
– Annual urine check for albumin: Microalbuminuria (30-300) gets ACEI and Statins right away
– ASA for macrovascular complications, NSAIDs for neuropathy
– Other goals: BP less than130/80, LDL less than 100, TG less than 150, HDL more than 40
– Dawn Phenomenon: Morning Hyperglycemia (8am glucose hi + 3 am glucose hi = incr evening dose)
– Somogyi Effect: Morning Hyperglycemia (8am glucose hi + 3 am glucose low = decr evening dose)
• Type 1: Insulin required to live, SQ in ab/butt/arm/leg; Regular insulin IV for emergency or
hospital maintenance; Can also add to TPN for maint
• Type 2: PO meds after diet and exercise have failed to increase sensitivity; Add insulin after PO meds have failed
– PO Hypoglycemics:
• Ex: Metformin (Glucophage)
– Lowers glucose absorption and production; hold prior to using IV contrast
– S/E: Hypoglycemia, Bloating, N/V/D
• Rosiglitazone (Avandia)
– Improves insulin sensitivity
– S/E: CHF/Edema, Hives, Anemia, Increased Cholesterol, Wt gain
Acute TX of poor glucose control
• DKA: (5-10% mortality)
– Almost exclusively in Type 1 diabetics
– S/S: Polyuria, dehydration, ab pain, fruity breath, AMS, low Na/Mg/Phos, hi K (but low total body), + following:
• Hyperglycemia (more than 250)
• Metabolic acidosis (pH below 7.3, HCO3 below 15, AG above 20)
• Ketonuria/Ketonemia
– TX:
• 1o: IV insulin bolus (0.1 unit/kg) then IV infusion with same amount per hr AFTER making sure pt is not low K
– Continue until acidosis corrects then taper
• 1oa: NS immediately upon diagnosis
– Switch to D5NS when glucose less than 250
• 2o: Add KCl to IV fluids once K less than 5; replenish other electrolytes as necessary
• Hyperosmolar Hyperglycemic nonketotic syndrome:
– Severe hi Glucose, almost exclusively in Type 2 diabetics
– Similar to DKA but usually have much higher glucose (above 600) and NO acidosis or ketonuria/emia
– Treat with fluids and low dose Insulin infusion
• Hypoglycemia:
– Patho: When glucose drops to 80 = insulin levels decr ; 70 = Glucagon incr; 50 = epinephrine incr along with signs such as sweat, hi BP, hi HR, tremors; Also around 50 CNS s/s (drowsy, h/a, confused) begin
– Note: S/S from epinephrine release are absent if pt is on a BB
– TX: If pt is alcoholic give Thiamine before any other treatment to prevent encephalopathy
• 1o: Can eat = hi sugar food; Can Not eat = 1/2 - 2 amps D50 IV push; (Glucagon alternative option if no IV access is available, however is of no use in prolonged hypoglycemia because stores of glycogen are depleted)





4 comments:
Thank you for sharing this information
Best Endocrinologist In Noida
I had my TL a little more than a year ago when my third child was born via c-section. I was not told ANYTHING about the possible side effects of having this procedure. Since then I have experienced heavy bleeding lasting sometimes 3 weeks out of the month, weight gain, severe mood swings. Severe cramping, changes to my libido, severe depression accompanied by suicidal thoughts, headaches, migraines, many new symptoms & older issues are now exacerbated. The father of two of my children doesn't want me anymore. I've become too much of a pain in the ass I guess. We don't talk. We don't sleep in the same bed. I think he might really think I am crazy... & maybe I am. I feel crazy a lot of the time.
I'm unpredictable. I feel so angry about the whole thing & now what was once a mild fear of doctors has exploded into full on white coat syndrome that causes me to have a panic attack/hypertensive emergency (severe increase in blood pressure) whenever I have to deal with them. I'm not sure what to do... I fear the next time I have to see a doctor I'll have a stroke or a heart attack from the stress & anxiety of it... what do I do? I take my time and keep searching on internet looking for natural healing that how I came across Dr Itua herbal center website and I was so excited when Dr Itua told me to calm down that he will help me with his natural remedy I put my hope on him so I purchase his herbal medicines which was shipped to my address I used it as prescribed guess what? I'm totally healed my cramp pain is gone completely I also used his Anti Bacteria herbal medicines it's works for me very well I want anyone with health problem to contact Dr Itua herbal center for any kind diseases remedies such as Parkinson, Herpes, ALS, MS, Diabetes, Hepatitis, Hiv/Aids,Cancers, Men & Women Infertility, I got his email address drituaherbalcenter@gmail.com he has any kind of herbal remedies for women & men also for our babes. I really miss my Hunni...he's a fantastic father & a good man. He doesn't deserve this. I feel like an empty shell of who I used to be.
I started on COPD Herbal treatment from Ultimate Life Clinic, the treatment worked incredibly for my lungs condition. I used the herbal treatment for almost 4 months, it reversed my COPD. My severe shortness of breath, dry cough, chest tightness gradually disappeared. Reach Ultimate Life Clinic via their website www.ultimatelifeclinic.com . I can breath much better and It feels comfortable!
Understanding how pharmacology interacts with endocrine diseases is crucial for effective treatment.
Post a Comment